Chinese Journal of Plastic Burn Surgery, Vol. 14, No. 5, Sep. 1998
Research and application of acellular allogeneic dermis and autologous thin skin sheet transplantation
Sun Yonghua, Li Chi, Wang Chunyuan, Qin Fengjun, Yu Dongning, Chen Zhong, Wang Rong, Hu Jie, Wu Yanan
【Abstract】
Purpose: To seek good covering materials for the repair of deep burn wounds.
Method: The allogeneic skin extracellular matrix was fixed and cross-linked with a fixative, and then the epidermis was removed with trypsin and EDTA chelating agent, the basement membrane was retained, and the cell components in the dermis that can trigger the host cell recognition response were treated with DNase, RNase and chemical agents, and the morphology of the intact basement membrane and extracellular matrix was retained to make a reticulated "acellular allogeneic dermis".
Results: Animal experiments (purebred Wister rats) proved that the transplant survival rate was high, there was no rejection, the shape and structure were intact 8 weeks after histological observation, the inflammation disappeared, the nail process was well combined with the acellular dermis at 12 weeks, and the collagen was neatly arranged. After first-degree wound and scar resection in 37 burn patients, acellular dermis + autologous thin skin slice (8‰ inch) transplantation was performed, and the average survival rate was 96.2% ± 3.4%. The wound shrinkage is light, the appearance is flat, the color is dark, the touch is soft, and the function is good.
Conclusion: Acellular homogeneous dermis + thin autologous dermal transplantation is an ideal material for repairing deep burn wounds.
【Keywords】 burns; Graft; Acellular dermis
After deep second-degree burn wounds heal or large-scale full-thickness burns, scab grafting or covering autologous epidermal cell culture with early scab grafting; or large allogeneic skin windows embedded in autologous miniature sheets; or autologous mesh skin grafting and autologous microparticle skin transplantation often have different degrees of scarring, and the appearance is uneven, painful and unbearable, especially in functional parts, which often lead to deformity and dysfunction. Previous treatments have shown that the thickness of the dermis contained in the transplanted skin is directly related to the degree of skin contracture, but the thicker the skin cut from the autologous donor area, the more severe the scar left in the donor area, and the more it cannot be cut repeatedly. In order to solve the difficulty of donating skin materials, scholars at home and abroad have focused on the research of composite skin [1~6], that is, a new type of burn wound covering or artificial dermis (Integra) and autologous epidermal transplantation formed by the combination of autologous epidermis and allogeneic dermis. We used the one-time surgical transplantation method of acellular allogeneic dermis and 10 autologous thin tomographic skin slices, and carried out animal experiments and preliminary clinical observations, in order to provide ideal permanent wound covering materials for clinical practice.
1. Materials and methods
1. Experimental animals: 80 purebred Wister rats, weighing 250~300 grams, provided by the Animal Experiment Center of the Academy of Military Medical Sciences.
2. Preparation of acellular allogeneic dermis: donor rats were fed separately 1 week before use, and 1 day before operation
Mao, intraoperative ether anesthesia, iodine alcohol routine disinfection, and towel. The full-thickness skin of the rat was cut, the subcutaneous tissue was cut off, and the extracellular matrix of the skin was cross-linked after rinsing with a large amount of disinfected normal saline using conventional fixative (20% formalin, etc.); Trypsin and EDTA chelating agents were used to remove the epidermis and preserve the basement membrane; Then use DNase, RNase, other chemicals, hypotonic compound buffer, EDTA chelating agent, etc. to treat the cell components in the dermis that can trigger the host cell recognition reaction, completely retain the morphological structure and components of the extracellular matrix, and use a special netting machine to form a fine net, and store it at 2~8 °C for later use.
3. Acellular allogeneic dermal test[7]:
3.1 Physical properties: elastic, bent without breaking, milky white, reticulated.
3.2 Histological structure: The structure of the dermal tissue is the same as that of the extracellular matrix structure in the normal human dermis. There is an intact basement membrane, no cells, no nucleus, and occasionally trace cellular debris.
3.3 The cytotoxic reaction of aseptic growth is not greater than grade 2. Intradermal stimulation (1). Irritation of the oral mucosa is no more than 1 point. Genotoxicity (Ames test) is (a).
4. Preparation of acellular allogeneic skin: ether anesthesia, hair removal, routine disinfection and towel laying on the day of surgery. Cut large
The rats were fully thick-skinned, rinsed with disinfectant saline 3 times, and set aside.
5. Composite Skin Grafting Surgical Method:
5.1 The animals were divided into acellular allogeneic dermal 10 autologous thin skin slice group (1 group) and non-decellularized allogeneic dermal 10 autologous thin skin slice group (2 groups).
5.2 64 rats, under ether open anesthesia, a full-thickness skin wound with a diameter of 3cm was excised above and below the back to fully stop the bleeding. Several pieces of thin tomocine skin were selected from the back of the rat for later use.
5.3 Group 1: Acellular allogeneic dermis was implanted into the wound surface of ten autologous thin tomotic skins, several stitches were sutured around the periphery, and dressings such as oil gauze and gauze were covered and bandaged and fixed (n= 32). Group 2: 10 autologous thin tomography of the wound surface implanted with acellular allogeneic skin
The skin and periphery were sutured with several stitches, and the dressings such as oil gauze and gauze were covered and bandaged and fixed (n=32).
5.4 Wound measurement with a scale for record [8]. Each experimental animal is cage fed. After 2, 4, 8, 12 and 24 weeks of postoperative observation, 6 animals were selected for each group to be killed alive each time, and 12 specimens (n=12) were taken for histological examination. 2 were left for long-term observation, and the longest survival was 11 months.
Second, the experimental results
1. Appearance: The thickness of the grafted area in group 1 was close to the normal skin thickness around the wound, and there was no obvious contracture on the wound surface. The wound contracture was more obvious after the fourth week of surgery in the second group without acellular allogeneic skin transplantation.
2. Skin survival rate: Except for being eaten by the rats themselves, the wounds all survived well. The average survival rate of 1 is 96.2% ± 3.4%, and the average survival rate of 2 is 90. 4%±1.2%。
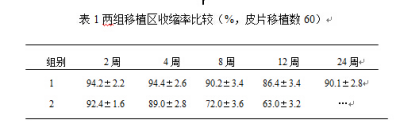
3. The wound shrinkage rate is shown in Table 1:
4. Histological observations:
4.1 2 weeks after acellular allodermal transplantation: the epidermis and allogeneic dermis survive, with more fibroblasts and capillaries in the dermis, macronuclear cells and inflammatory cells.
4.2 4 weeks after transplantation: the morphology of the allogeneic dermis is close to normal, most of the capillaries grow vertically in the epidermis, there is inflammatory cell infiltration, and there is a keratinized layer.
4.3 8 weeks after transplantation: the morphology of the allogeneic dermis was normal, and there was no obvious inflammatory reaction. 12 weeks post-transplantation: normal dermal tissue morphology with a small number of nail processes in the epidermis. 24 weeks after transplantation: normal skin tissue, structurally intact, no skin appendages, no rejection. The longest surviving rat was 11 months, and the biopsy results were the same as those at 24 weeks after surgery.
5. Summary: Allogeneic dermal transplantation can survive, has low antigenicity, and can induce cell and epithelial growth. The combination of allogeneic dermis and grafted epidermal tissue results in a good appearance with light contractures.
3. Clinical application
1. Observation content: the survival rate of acellular allogeneic dermis after skin grafting, scar growth after wound healing, wound shrinkage rate and function, etc.
2. Surgical methods: 37 adult inpatients with fresh third-degree burn wounds and adult patients with post-burn scar deformity were selected from May 1996~February 1997. The prepared acellular allogeneic dermis was transplanted with ten autologous thin layers of skin (about 8‰ inches of thin skin were cut with a Zimmer electric skin extraction machine or a roller peeling knife) for transplantation, and after the wound was covered with oil gauze, the multi-layer dressing was moderately pressurized and bandaged. During the operation, attention should be paid to aseptic operation, the wound base should be fully hemostated, and sterile saline should be irrigated. Generally, the wound is examined 10~14 days after surgery.
3. Observation method and result evaluation: The wound was observed at 2.4, 8 and 12 weeks after surgery, and the color, hardness and elasticity were observed. The survival rate of skin grafting was measured with a wound measuring scale [8], and the intersection of skin graft area and original area was measured at 4, 8, 12, 24, and 48 weeks after injury, and the skin shrinkage rate and other values were calculated, and the t-test analysis of variance was statistically treated.
4. Results:
4.1 Skin survival rate: Except for 1 case of 41 wounds transplanted in 37 patients, the skin slice did not survive due to acellular allogeneic subdermal hemorrhage, and the rest of the wounds survived well, with an average survival rate of 96. 2% and 3.4%.
4.2 The wound shrinkage rate is shown in Table 2.
4.3 The appearance is flat, there is no scar hyperplasia, the color is still dark, the touch is soft, and the functional parts function well.
5. Typical Cases:
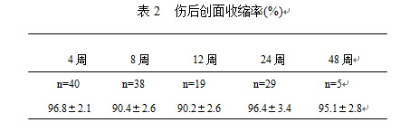
Example 1: Male, 40 years old. On May 27, 1996, due to a coma after alcoholism, both lower limbs soaked in hot boiled water, rescued after being discovered, both lower limbs, buttocks, especially the left lower limb were third-degree burns, feet, ankles, and most of the lower calf bone cortical necrosis, after admission to the hospital, necrotic tissue excision, part of the autologous skin grafting, the buttocks and the upper lateral side of the left knee were selected for J-1 acellular allogeneic dermal transplantation, which was covered with autologous thin tomographic skin, 2 weeks after the operation, all the skin grafts survived, half a year after the operation, the healing wound was flat, smooth and functional, The complexion is close to normal (Figs. l~3).
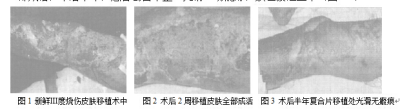
Case 2: Male, 20 years old, was admitted to the hospital on May 23, 1996 due to gas burns on his face and upper limbs, with an area of 20% and grade III. On the morning of May 27, both upper limbs were crusted under general anesthesia, thin tomodermal skin was removed from both thighs, and J-1 acellular allogeneic dermal transplantation was performed on both forearms, which were covered with autologous thin tomotic dermapace, and part of it was only autologous thin tomotic reticular skin transplantation. At 5 weeks after surgery, the wound skin was well viable, and at 12 weeks after surgery, a small prominent scar growth was visible at the simple tomotic reticuloderm graft site, the composite skin graft site was smooth and flat, the cells in each layer of the epidermis were intact and there were nail processes on the surface by light microscopy, a small number of inflammatory cells in the superficial dermis were infiltrated, and there were coarse collagen and fibroblasts in the deep dermis, and no skin attachments were found (Figs. 4 and 5).
4. Discussion
1. In 1913, Loewe [9] successfully applied dermal grafting for the first time. Dermal tissue not only enhances the toughness of the grafted skin, but also inhibits granulation tissue growth and scarring, and reduces wound shrinkage. The use of composite skin grafts to repair tissue damage caused by deep burns or trauma, reduce scarring, and improve function has been widely reported. Cuorio [10] planted allogeneic dermis preserved with liquid nitrogen and freshly cut the scab wound after burns, and after 3~5 days, the dermis was removed after the dermis established blood vessels, and then the cultured autologous keratinocyte membrane was transplanted on the allogeneic dermis. Mekay et al. [11] treated with DispaseII., glycerol-preserved allogeneic dermis, and preliminary clinical application showed less scarring after survival. Wain Wright [5] reports cell-free allodermal deca-reticulo-autologous thin-dermal transplantation. Tompkins et al. reported [3]Integra (trade name) is a double-layer artificial skin with a three-dimensional structure similar to that of normal dermis, which provides three-dimensional structural information to ingrown fibroblasts and induces fibroblasts to synthesize nascent connective tissue with a dermal structure. Chen Bi reported [12] that piglets were used as animal models, and allogeneic lyophilized dermis, pancreatic treated allogeneic dermis and fresh allogeneic dermis were used to transplant autologous derm on top of it.
The animal experiments and clinical results of this group showed that the survival rate of acellular allogeneic dermis and autologous thin dermal tablets was high at the same time. Histological observation 2 weeks after transplantation showed the presence of inflammation, which increased with the duration of transplantation
Gradually disappearing, the collagen is arranged neatly, and a particularly prominent feature is that it has a complete basement membrane, and the autologous epidermal cells covering the basement membrane surface have firmly integrated with the decellularized dermis, and continue to expand and thicken the epithelium.
The results of this experiment support the important role of basement membrane in wound healing reported by Chetty [13] in 1992, and the fragility and blistering of the skin after transplantation reported by Compton and O'Connor et al. [14] in 1989 due to the lack of basement membrane.
2. Acellular allogeneic dermal transplantation is applied, and the preservation of the extracellular matrix can guide cell regeneration and expansion, promote the growth of autologous fibroblasts in the allogeneic dermal scaffold, and promote wound healing. Both Takami [15] and the method in this experiment were able to completely remove allogeneic intradermal cells and preserve the allogeneic dermal structure.
3. In 37 clinical patients, 41 wound transplantation cases were observed, and the survival rate of acellular allogeneic dermal composite transplantation was 96. 2%±3.4%, smooth appearance and good function. The acellular allogeneic dermis retains the matrix as a framework, and has an intact basement membrane to create a good foundation for the survival of the autologous epidermis and the connection between the dermis and the epidermal layer. At the same time, due to the absence of epidermal cell components and low tissue antigenicity, the skin piece can survive for a long time, the donor skin area is less damaged, the recovery is fast, and there is no scarring, which is a good wound covering for repairing deep burn wounds and has broad application prospects.
References
1. Burke JF, Yannas IV, Qurn WC, et a/. Successful use of a physioloically acceptable artificial skin in the rreatment of extensive burn injury. Ann Surg, 1981,194:413.
2. Bell E, Ehrlish HP, Batten DJ,etal.Developement and use of living skin eqivalent. Plast Reconstr Surg, 1981,67:356.
3. Tompkins RG, Burke JF. Progress in burn treatment and the use of artificial skin. World J Sarg, 1990,14:819.
4. Yannas IV, Lee E,Qrgill DP,etal.Synthesis and eharacterization of a model extracell-uar metrix that induces partial regeneration of adult mammaliam skin. Proc Natl Acad Sci, 1989, 86:933.
5. Wain Wright DJ. Use of an acellular allograft dermal maxtrix (Allodermal) in the management of fullthickness burns. Burns, 1995, 21:243-248.
6. Soejima K, Nozaki M, Sasaki K, et a/. Reconstruction of burn deformity using artificial dermis combined with thin split-skin grfting. Burns, 1997, 23:501-504.
7. International Standard:Biological evaluation of medical devices part l.Guidance
on selection of tests. ISO. 1993-1.
8. Li Chi, Sun Yonghua. Measuring tape for small burn wounds. Chinese Journal of Plastic Burn Surgery, 1992, 8:241-242.
9. Loewe 0. Uber Hautimplantation on stelleder Freien Faszienplastik. Plast Reconst Surg. 1960, 26:1.
10. Cuono CB. Composite antologous-allogeneie skin replacement:development and clinical application. Plast Reconstr Surg, 1987, 80:626-635.
11. Mekay I,Woodward B,Wood K, et al. Reconstruction of human skin from glycerol preserved allodermis and cultrued keratinoeyte sheets. Burns,1994, 20:19-22.
12. Chen Bi, Tang Chaowu, Gong Xirong. Experimental study of composite skin grafting. Chinese Journal of Plastic Burn Surgery, 1990, 7:29-30.
13. Chetty BV, Boissy RE, Warden GD, et al Basement membrane and fibroblast aberration in blisters at the donor, graft and spontaneously healed sites in patlents with burns. Arch Dermatol, 1992, 128:181-186.
14. Compton CC, Gill JM, Bradford DA,etal. Skin regener-ated from cultured epithelial autografts on full-thicknessburn wounds from 6 days t0 5years after grafting A light,electron microsopic and immunohistochemical study. LabInvest, 1989, 60:600-612.
15. Takami T, Matsuda M,Yoshi take, et al. Dispase detergent treated dermal as a dermal substitute. Burns, 1996,22:182-190.
(Received:1997-12-28)